The migraine and other headaches pathway is intended for use by clinicians as a guideline for managing patients with acute severe headache.
Pathway flowchart
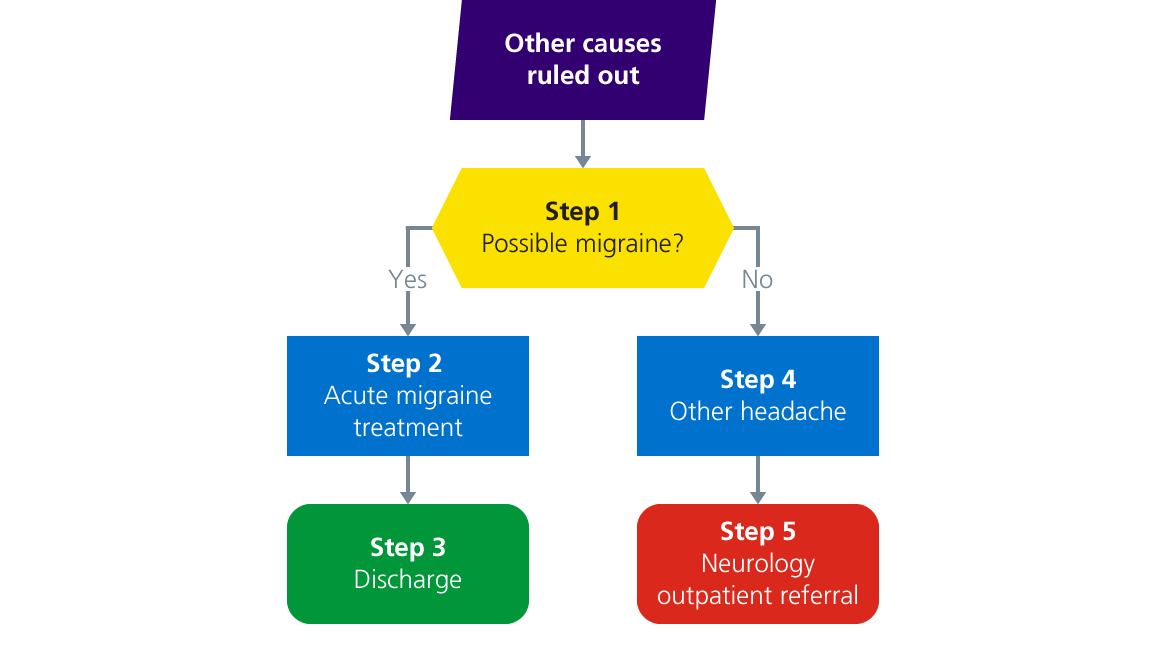
Pathway description
Step 1: migraine?
Migraine summary:
- People with migraine want to go somewhere quiet and lie down
- Offer acute treatment (no codeine) – most can be discharged within 48 hours
- Consider prophylactic treatment or give advice to primary care
- Only refer to Neurology if refractory to three prophylactic agents
When secondary headaches and other forms of primary headache syndromes have been excluded the final diagnosis is usually migraine with or without aura.
The key feature of migraine is that patient will want to go and lie down when the headache is at its worst. It can sometimes be difficult to extract from people that this is the case.
If patients have headaches every day, ask about whether there are some days where the headache is so bad the need to lie down. If the patient is very busy (young children, busy job etc.) ask what they would do in an ideal world.
Next steps:
- If yes, proceed to step 2
- If no, proceed to step 4
Step 2: acute migraine treatment
The key feature of this is that patients will want to go and lie down (the opposite of raised intracranial pressure).
The treatment for an acute severe migraine is:
- High dose NSAID of your choice provided there is no contra-indication (diclofenac 50mg oral or IM TDS)
- An antiemetic which improves stomach emptying (domperidone 10mg TDS)
- A triptan of your choice provided there is no contra-indication (sumatriptan 50mg BD)
- IV fluids (3x8 hourly 1L bag normal saline)
- +/- paracetamol 1g QDS +/- diazepam 10mg as a once off treatment if the patient is extremely distressed
Codiene makes migraines worse in the long term, so is best avoided unless there is no other option (this goes for all opioids).
Proceed to step 3.
Step 3: discharge
We have some well-established and evidence based guidelines for the management of migraine in primary care and it is reasonable to give those to the patient and/or GP on discharge.
We no longer have the wherewithal to see the majority of migraine patients in Neurology. There are well validated guidelines for the management of migraine in the community if you are confident to initiate that.
Step 4: other headache
Cluster headache
- Cluster headaches and associated conditions are extremely unpleasant
- Key feature is that they are side-locked (always on the same side) and associated with autonomic activation, chiefly agitation – so the patient will pace about rather than lying down
- Acute treatment for cluster headache is high flow oxygen and subcut sumatriptan 6mg
- There are standard guidelines for managing cluster headache
- Please do refer these patients to urgent outpatient Neurology via email
- Be aware that acute glaucoma can be mistaken for cluster headache so, if the patient has unilateral blurred vision and a red, painful eye, please get advice from ophthalmology
Trigeminal neuralgia
Trigeminal neuralgia must be:
- limited to just the distribution of the trigeminal nerve and doesn’t radiate past the tragus of the ear or the inferior border of the mandible
- triggered by light touch on the face or teeth
- respond to carbamazepine, although the side-effects may make it difficult to tolerate. Please see the anti-seizure medication escalation guidelines for further details
If you think the patient has a new presentation of trigeminal neuralgia then please refer to urgent outpatient Neurology.
Tension type headache
- Tension type headache is present for long periods of time. It can feel like a tight band around the head.
- It can be triggered by musculoskeletal problems in the neck (you can feel the patient's neck and find that the muscles are very stiff), or dehydration
- Suggest neck exercises as outlined in the Chartered Society of Physiotherapy (CSP) videos
Medication overuse headache
- This commonly complicates migraine and tension type headache
- If the patient is taking any analgesic for more than 15 days a month, tell them to stop if they want the headache to go away
Step 5: Neurology outpatient referral
If the patient has tried and failed three prophylactic agents they can be referred to specialist Headache Clinic. In the referral you will need to include which medications have been tried and the reason for discontinuation.
We are keen to see other rare primary headache patients, please refer them for follow up.
Last reviewed: 24 January 2025