The thunderclap headache pathway is intended for use by clinicians as a guideline for managing patients with acute severe headache.
Thunderclap headache is the signature presentation for subarachnoid haemorrhage (SAH), although the number of people who present with just headache symptoms is relatively small.
A thunderclap headache is caused by the sudden introduction of blood into the subarachnoid space. Pain is hyper acute and increases from ‘no pain’ to maximum intensity in a matter of a few minutes.
CT scans have an extremely high sensitivity for SAH if completed within six hours of the onset of pain and interpreted by a neuroradiologist. CT scan sensitivity decreases after more than six hours, so a lumbar puncture (LP) may be required after this time frame.
A small SAH may be difficult to see and can be missed if you are not and expert. SAH is not the only cause of thunderclap headache so other causes should be considered.
Pathway flowchart
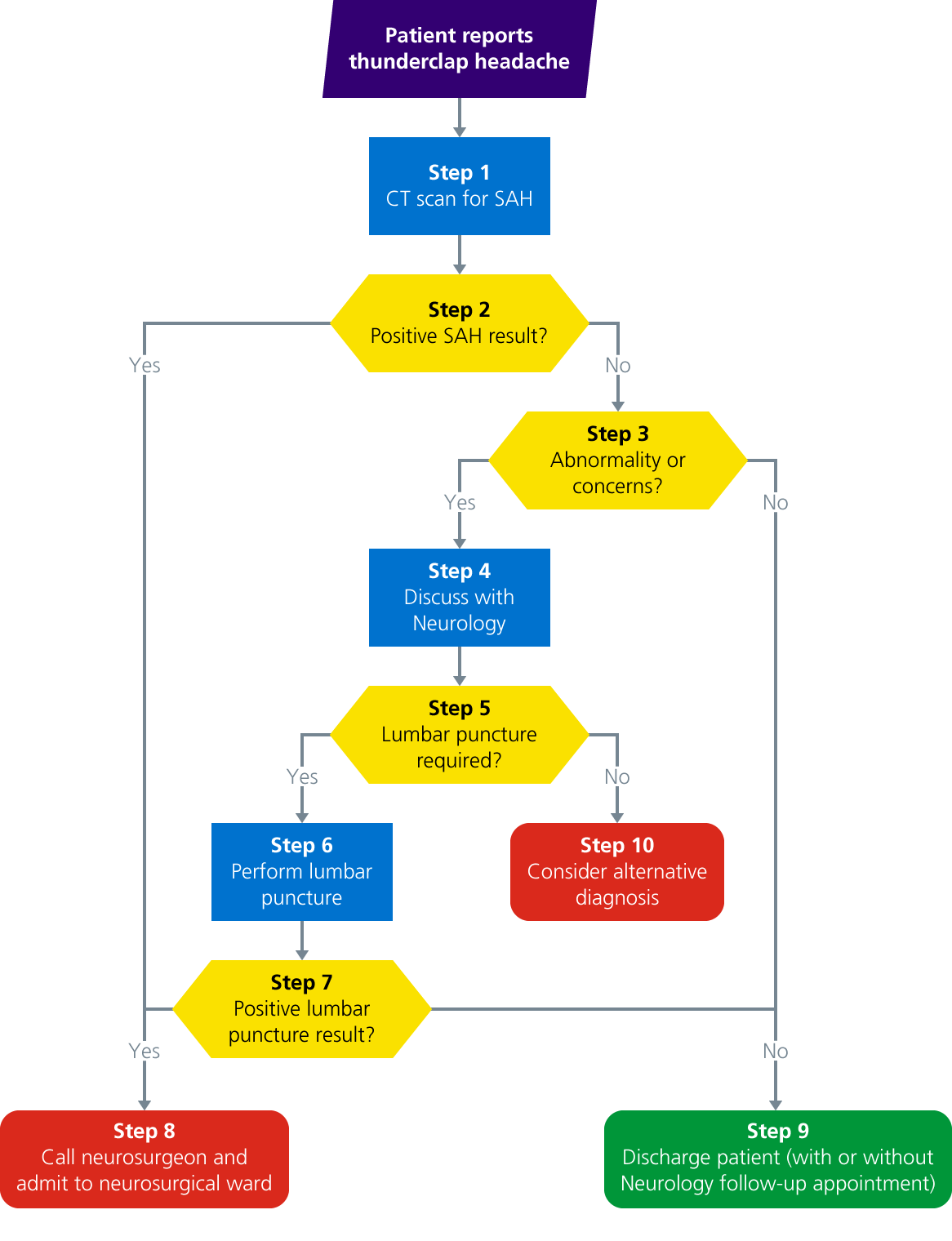
Pathway description
Step 1: CT scan for SAH
The key study by Perry et al. (2011) scanned 3,132 patients for thunderclap headache. Of the 953 patients that were scanned within six hours of the onset, 121 had a SAH.
All of the SAH patients had visible blood on their CT scans and none of the patients with a normal scan had blood detected in CSF, yielding 100% sensitivity, but there are caveats:
- Sensitivity for patients who were scanned six hours after the onset of pain (which was the majority) was high but not 100%
- SAH can be very difficult to see and can be missed
- SAH is not the only cause of thunderclap headache, it can also be caused by:
- Pituitary apoplexy (should show up on the CT scan)
- Meningitis (would expect pyrexia, neck stiffness and abnormal CSF)
- CVST (ask the patient about pain getting worse on lying down or risk factors)
- Spontaneous dural tear (ask the patient about pain getting worse on standing up)
- If the patient has had recurrent thunderclap headaches, think of RCVS
Please note: if the scan was done six hours after the onset of the headache you cannot use it to definitively exclude a SAH.
After performing the CT scan for SAH, proceed to step 2.
Step 2: positive SAH result?
- If yes, blood is visible on the CT scan, proceed to step 8
- If no, proceed to step 3
Step 3: abnormality or concerns?
- If yes, proceed to step 4
- If no, proceed to step 9
Notes
- CT scans have an extremely high sensitivity for SAH if completed within six hours of the onset of pain and interpreted by a neuroradiologist
- CT scan sensitivity decreases after more than six hours, so an LP may be required
- A small SAH may be difficult to see and can be missed if you are not an expert
- SAH is not the only cause of thunderclap headache so other causes should be considered
Step 4: discuss with Neurology
If another abnormality is visible on the CT scan or you are concerned, you may need to discuss the case with the neurology or cranial neurosurgery SpR. We would expect plain CT to show some other serious causes of thunderclap headache (pituitary apoplexy), but some causes may not show up on plain CT such as:
- Meningitis
- CVST
- Spontaneous dural tear
If SAH cannot be excluded on the CT scan or you are concerned about another secondary headache, the patient may need an LP. You may wish to discuss this with the neurology SpR first.
In working hours the neurology team may be able to reverse the diagnosis of a thunderclap headache and avoid the need for an LP.
A neurology SpR and consultant are available by phone 24 hours a day. At weekends and out of hours the Neurology team provide non-resident 24 hour cover, so please try not to call with routine enquiries about stable patients at unsociable hours.
The neurology ward has limited bed space and no on-site middle grade cover out of hours. Where possible, it is preferable to not admit patients directly to the ward after 17:00.
After discussion with Neurology, proceed to step 5.
Step 5: lumbar puncture required?
- If yes, proceed to step 6
- If no, proceed to step 8
Step 6: perform lumbar puncture
- Before performing a lumbar puncture you need to wait over 12 hours from the onset of the headache
- Measure the opening pressure
- Mark on the bottles the order in which they were collected
- Send the CSF for bilirubin
- Protect the sample from light
- Make sure the CSF is also sent for protein, cell count and glucose (collect last CSF sample in grey top tube and send blood glucose with the sample)
After performing the LP, proceed to step 7.
Notes
CSF bilirubin is the marker of a SAH. Bilirubin is only generated in vivo, which means that if found, the blood must have been in the CSF before the LP needle was inserted. Blood in the CSF can break down to oxyhaemoglobin in vitro, so does not help.
If the CSF is not protected from light the bilirubin can deteriorate and the test can be missed. If the CSF is heavily blood stained then it can be difficult to detect bilirubin, which is why you need to label the CSF sample bottles with the order in which they were collected.
The number of red cells should be the same in all three bottles with a SAH, whereas is if the blood has come from an epidural vein which has been punctured during the procedure, the number of red cells should go down with each successive bottle.
Other causes
LPs can be used to rule out other causes of secondary headache:
- CVST will have a high opening pressure (>20cm of water)
- CSF hypotension with have low opening pressure (<7cm of water)
- Meningitis will have a high white cell count and, depending on the type, a very low CSF glucose. This needs to be compared to the blood level so you need to send a blood sample at the same time. For glucose the CSF needs to go to the lab in a grey top tube
If the opening pressure is high and the rest of the constituents of the CSF are normal then consider screening for and possibly treating IIH.
Step 7: positive lumbar puncture result?
- If yes, proceed to step 8
- If no, proceed to step 9
Step 8: call neurosurgeon and admit to neurosurgical ward
- Positive SAH result: contact the on call cranial neurosurgery SpR via switchboard and discuss admission to Neurosurgery
- Positive LP result: the patient will need to be discussed with the Neurosurgical team if there is CSF bilirubin in the CSF. In almost all circumstances the patient will need to be admitted for an angiogram
Step 9: discharge patient (with or without Neurology follow-up appointment)
If you are happy that a secondary headache has been excluded, the patient is safe to be discharged. Make sure you offer the safety net of representing if things deteriorate or fail to improve.
We can no longer see the majority of migraine patients in Neurology. There are well validated guidelines for the management of migraine in the community, so if you are confident you can
initiate that.
If the patient has tried and failed three prophylactic agents they can be referred to specialist headache clinic. In the referral, you would need to include which medications have been tried and the reason for discontinuation.
We are keen to see other rare primary headache patients, please refer for follow up.
Step 10: consider alternative diagnosis
- You need to think about other causes of secondary headache
- Many will be excluded on the plain CT scan but you may need to consider a CTV or LP
- The most serious and common causes are meningitis and CVST
Last reviewed: 06 September 2024