The raised intracranial pressure pathway is intended for use by clinicians as a guideline for managing patients with acute severe headache.
Pathway flowchart
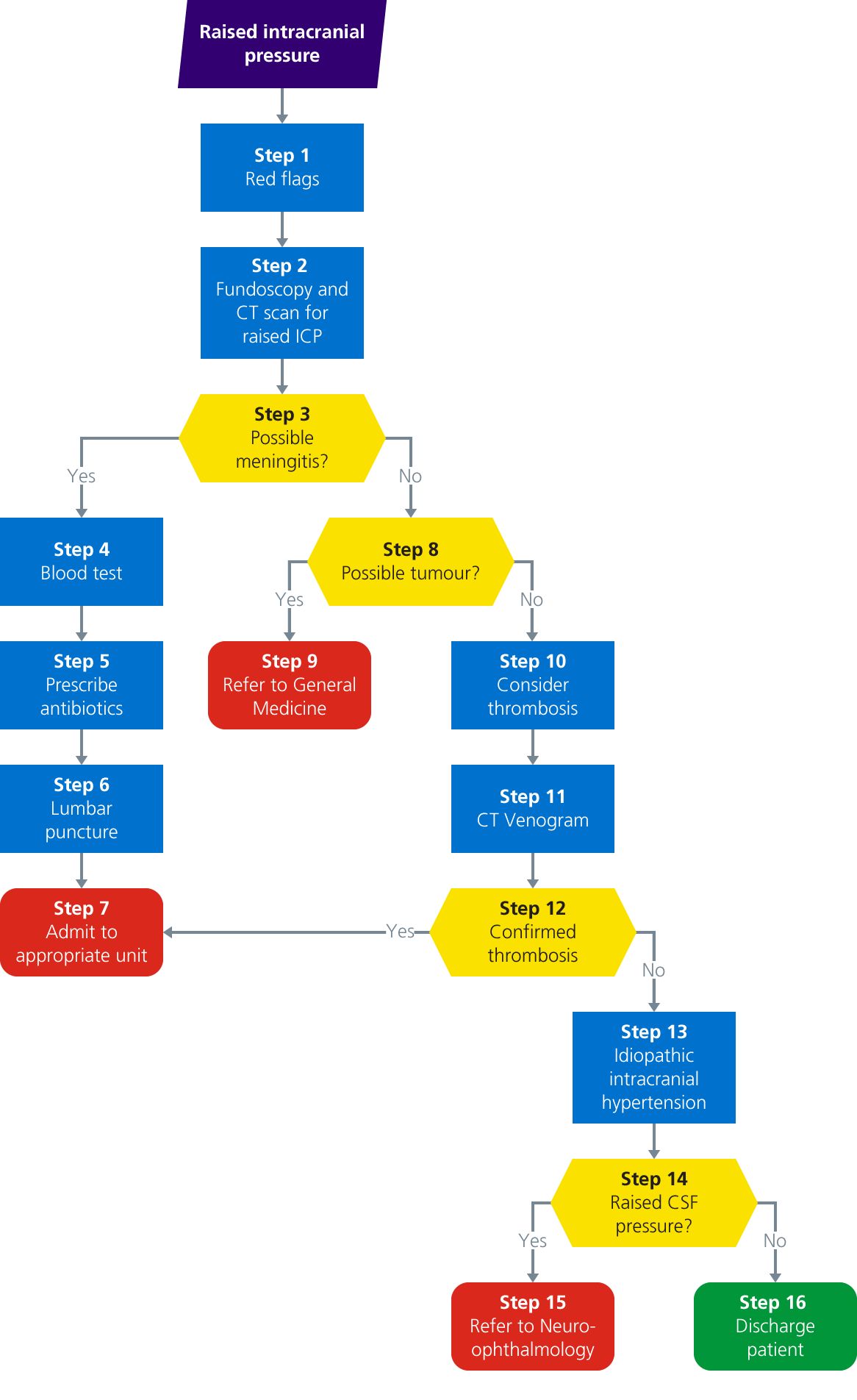
Pathway description
Step 1: red flags
Ask the patient about the following red flags:
History of cancer or HIV
- The most common type of brain tumour is a metastasis. If someone has a history of cancer in the last five years and a new headache, they need a scan
- People with HIV which is undiagnosed, untreated or with a low CD4 count are at increased risk of space occupying lesions such as TB, cysticercosis, toxoplasmosis and B-cell lymphoma
- Anyone with HIV and a new headache needs a scan
Pregnant or just gave birth
- Pregnant women or patients who have just given birth are slightly immunosuppressed and are at a slightly higher risk of listeria. They are also somewhat hyper-coagulable, so CVST is more prevalent in this group
- If there has been a spike in BP then pre-eclampsia or eclampsia can occur. The presentation is very similar to PRES/RCVS. You will need to ask about booking BP as a jump to 150 systolic from a pre-pregnancy level of 90 systolic can trigger vasospasm
Focal neurological deficit
- Often people with migraine will have focal neurological symptoms
- Symptoms are more likely to be positive (tingling or flashing lights) and progressive (related to a wave of excitation which crosses the cortex over about 15 to 30 minutes) than in a stroke (almost always a deficit with sudden onset caused by the suddenly blocked or ruptured artery)
- Strokes can also cause migraines. If this is the first time it has happened or if it is much more prolonged than usual, it is sensible to keep the patient in and scan them
- Ischaemic strokes and TIAs are caused by embolization of an unstable thrombus. This means you don’t tend to get lots over a prolonged period; either people have a bunch of TIAs within the space of a day and then have a stroke or they will get one TIA and then have the stroke within a couple of weeks. This is the reason that TIA clinics are done the next day
Seizures
- All first seizure patients need a CT and referral to the ‘first-fit clinic’
Cognitive impairment or personality change
- Rapidly progressive dementia is one of the more common presentations of brain tumours
- Do listen to the family; if they say the patient has changed significantly then they need a scan
Pain gets worse on lying down
- The key feature of migraine is that a patient will want to go and lie down when the headache is at its worst. It can sometimes be difficult to extract from people that this is the case
- If a patient has headaches every day, ask about whether there are some days where the headache is so bad they need to lie down
- If the patient is very busy (young children, busy job etc.), ask what they would do in an ideal world
- If pain gets worse on lying down it suggests raised ICP (which needs to be excluded) or mechanical neck pain
Blurred or altered vision
- Look for or ask about loss of visual fields, loss of colour vision, flashing lights on Valsalva or vision ‘going black’ on Valsalva
- Try to differentiate from migraine aura (flashing lights and/or a black cloud) which spreads across the visual field over the course of about 25 to 30 minutes
Pain is at its worst immediately on waking or it wakes patient from their sleep
- This sometimes implies raised ICP, the increase in blood flow overnight can trigger a headache
- It is worth noting that cluster headache also has a habit of waking people from their sleep
Pain on bending or Valsalva
- This is not terribly helpful. It is more usually ‘mechanosensitivity’ - the stiff, painful neck which is a feature of a migraine
- If a headache comes on immediately after Valsalva (cough, cough, cough, tiny pause, headache) this may be a marker of symptomatic Chiari malformation and it would be reasonable to get a scan to look for this
After checking for red flags, proceed to step 2.
Step 2: fundoscopy and CT scan for raised ICP
Fundoscopy
You must attempt a fundoscopy to look for papilloedema.
CT scan
Radiologists will say that you can’t exclude raised ICP with a CT scan. However, you can look for space occupying lesions, hydrocephalus or obstruction of the CSF pathways.
It is worth checking with the radiologist who reports the scan to check that there is no visible contra-indication to LP.
Raised ICP is not a contra-indication in its own right to LP as patients with IIH have raised ICP.
It is crucial that the CSF pathways are open and there is no space occupying lesion which will result in a pressure differential between the intracranial space and the spinal CSF space which could result in ‘coning’.
After performing a fundoscopy and CT scan for raised ICP, proceed to step 3.
Step 3: meningitis?
The patient will be pyrexial and have neck stiffness. If the patient is also confused or has had a seizure then consider viral encephalitis.
This is clearly a medical emergency. Follow the meningitis section of 'adult guidelines for antimicrobial prescribing' Trust protocol (see downloads section) or view the NICE guidelines (see other websites section).
- If yes, meningitis is possible, proceed to step 4
- If no, proceed to step 8
Step 4: blood test
- Antibiotics are started as a priority with patients with possible meningitis
- The patient should have an LP as soon as it is safe to do so (CT to exclude obstructive hydrocephalus)
- The LP is often done a few days later, by which time the levels of bacteria in the CSF may be too low to culture. However, it should still be done
- It is very helpful to have blood cultures done before or very shortly after giving the antibiotics
- CRP is sensitive for bacterial meningitis. A normal CRP would not exclude meningitis, but is very re-assuring if the pre-test probability of bacterial meningitis is felt to be low
After performing a blood test, proceed to step 5.
Step 5: prescribe antibiotics
- If meningitis is suspected the ‘door to needle time’ for antibiotics is crucial
- Follow the 'adult guidelines for antimicrobial prescribing' Trust protocol (see downloads section), prescribe the antibiotics as the top priority and don’t leave the vicinity of the patient until the antibiotics are up and running
- Note that until you know what the causative agent is, the patient is assumed to benefit from dexamethasone
After prescribing antibiotics, proceed to step 6.
Step 6: lumbar puncture
- Opening pressure should be measured. This can flag up things like CVST and cryptococcal meningitis
- Make sure the CSF for microscopy, culture protein, cell count and glucose is completed
- Collect the last CSF sample in a grey top tube and you will need to send blood glucose with the sample
Proceed to step 7.
Notes
- The presence of a contraindication on the brain scan or a coagulopathy due to sepsis may preclude an LP. If it is safe to do so, an LP is extremely helpful and the earlier it can be done the better
- Antiplatelets and anticoagulant treatment may need to be paused prior to doing the LP
- The LP can be used to rule out other causes of secondary headache:
- CVST will have a high opening pressure (>20cm of water)
- CSF hypotension with have low opening pressure (<7cm of water)
- Meningitis will have a high white cell count and depending on the type, a very low CSF glucose – this needs to be compared to the blood level so you need to send a blood sample at the same time. For glucose the CSF needs to go to the lab in a grey top tube
- If the opening pressure is high and the rest of the constituents of the CSF are normal then consider screening for and possibly treating IIH (although cryptococcal meningitis can also do this)
Step 7: admit to appropriate unit
- If you strongly suspect bacterial meningitis or you are concerned about severe sepsis or airway safety, please discuss the patient with the critical care team
- Admit the patient and discuss them with Infectious Diseases Team and/or Neurology
- There is a an ID and Neurology SpR, plus a consultant available by phone 24 hours a day
- Out of hours and at the weekend, the two teams are on a 24 hour non-resident, so please try not to call them with routine enquiries about stable patients at unsociable hours
- Many people with meningitis will need to be managed in critical care
- Always complete a HIV test (unless the patient is known to have HIV, in which case they need a CD4 count)
Step 8: tumour?
- If the brain scan shows a possible tumour, the patient will need to be admitted, investigated and discussed at the neuro-oncology MDT (every Tuesday morning)
- It is better not to tell the patient the lesion is a tumour unless you have done an MRI and have confirmation from a neuro-radiologist. In most cases the neuro-oncology MDT will require an MRI scan with contrast
- Many brain tumours are metastases and most patients will require a CT of the chest-abdomen-pelvis
- Many patients will need a biopsy which may be done when the patient is an inpatient but may be arranged for a later date
- As you can imagine this is an extremely stressful time for the patient, the best that you can do is to be clear about the pathway:
- Scan
- Possibly a scan of the rest of the body
- Discussion at MDT
- Meet with the surgeon
Next step:
- If yes, proceed to step 9
- If no, proceed to step 10
Step 9: refer to General Medicine
- Refer to General Medicine and await a biopsy
- The on call cranial neurosurgery registrar is available via switchboard and will advise on the next steps
- It is most likely, given the pressure on neurosurgery beds, that the patient will be admitted to a different ward
Step 10: consider thrombosis
Venous sinus thrombosis (CVST) is associated with raised intracranial pressure so the headache may get worse on lying down. Ask about risk factors:
- Thrombophilia
- Pregnancy or recent delivery
- severe anaemia
- dental or ENT infection
- AZT COVID vaccine
Proceed to step 11.
Step 11: CT venogram (with contrast)
- Prior requesting a CTV please make sure the case has been reviewed by a senior clinician or discussed with the Neurology team
- The CVST may be visible on plain CT, but may you may require a CT venogram (CTV) to exclude it
- This needs to be discussed with the on call radiologist
- You will need to make sure the patient has normal renal function (U+E blood test) and there are no allergy concerns
After completing a CTV, proceed to step 12.
Step 12: positive result?
For positive results:
- Admit to hospital
- Discuss with Neurology if possible
- Anti-coagulate with low molecular weight heparin (Clexane) unless contra-indicated
- Make sure the diagnosis is correct – get scan reported by a neuroradiologist
- Make sure you think about the eyes
- Perform fundoscopy and request review by ophthalmology to exclude papilloedema
- Ideally before starting LMWH (although do not delay treatment)
Next step:
- If yes, the result shows CVST, proceed to step 7
- If no, the result was negative, proceed to step 13
Notes
- CVST often is not as bad as you would think, however they can lead to seizures, venous cerebral infarcts, lobar haemorrhages, blindness and in severe cases raised ICP and death
- It is important the patient is stabilised and started on treatment before discharge
- If possible talk to the on call neurology team as soon as possible. If the CVST is in the context of heparin induced thrombocytopenia the outcome can be much worse and the treatment is different so it is better to discuss things
- For all other CVST the treatment is ‘treatment dose’ low molecular weight heparin even when there is an established haemorrhage. The heparin breaks up the clot a bit bringing the venous pressure down and reduces the risk of further deterioration
- Venous flow on MR scans can sometime appear to be blocked by something called arachnoid granulations or slow flow in hypoplastic transverse sinuses, these are both benign situations
- It is important that the scans are reviewed by a neuroradiologist and the diagnosis verified before the patient is committed to a prolonged period of anti-coagulation
- CVST can lead to sight threatening papilloedema; please consider referring the patient to ophthalmology for a safety check
Step 13: idiopathic intracranial hypertension
Idiopathic intracranial hypertension (IIH) is a condition where a patient produces too much CSF. To make the diagnosis the patient must have:
- Papilloedema
- Raised CSF opening pressure on LP done with the patient lying down. The standard upper limit of normal is 20cm of water, however we find that patients who are under stress sometimes have higher pressures than this. Also if the LP is done with the patient seated the pressure will be higher
- Normal CSF cell count, glucose and protein
It tends to occur in young women with a higher body mass index. It is associated with a headache that gets worse on lying down and visual disturbance; of which an actual loss of acuity is a late and emergency sign.
If you are not sure whether or not there is papilloedema you may be able to get optical coherence tomography or advice from Ophthalmology.
Proceed to step 14.
Step 14: raised CSF pressure?
- If yes, proceed to step 15
- If no, proceed to step 16
Step 15: refer to Neuro-ophthalmology
- Optical Coherence Tomography is a type of non-invasive retinal scan and may be available during working hours to assess objectively for papilloedema
- Before doing an LP in a suspected case of IIH it may be worth talking to neuro-ophthalmology to see whether it is possible to have the patient formally assessed or get OCT
- Neuro-ophhthalomology have an on call service, but it is ‘supra-regional’ and not available out or hours or at the weekend. In this case it is sensible to discuss with neurology or ophthalmology instead
- Once the patient has an established diagnosis of IIH then they will need to be discussed with neuro-ophthalmology anyway
- If there is sight threatening papilloedema then the patient should not be discharged until a management plan (usually involving CSF diversion surgery by a neurosurgeon) is in place
- If sight is not under threat then the patient will need monitoring by the neuro-ophthalmology team
Step 16: discharge patient
Try to make a diagnosis of a primary headache syndrome.
Last reviewed: 17 December 2024